Today i am talk about "what is cardiovascular system function"
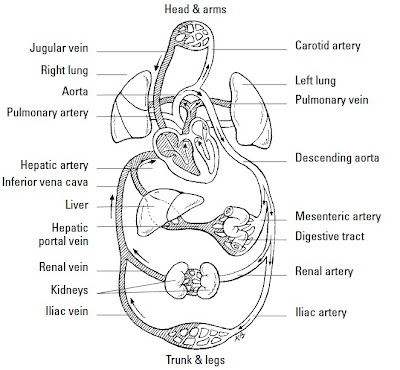
Moving to the Beat of a Pump Also called the cardiovascular system,
the circulatory system includes the heart, all blood
vessels, and the blood that moves endlessly through it all . It’s what’s
referred to as a closed double system; the term “closed” is used for three reasons: because
the blood is contained in the heart and its vessels; because the vessels specifically target the
blood to the tissues; and because the heart critically regulates blood flow to the tissues.
The system is called “double” because there are two distinct circuits and cavities within the
heart separated by a wall of muscle called the septum. (Each cavity in turn has two chambers
called atria on top and ventricles below). The double circuits are the following:
1. The pulmonary circuit carries blood to and from the lungs for gaseous exchange.
Centered in the right side of the heart, this circuit receives blood saturated with
carbon dioxide from the veins and pumps it through the pulmonary artery (or trunk)
to capillaries in the lungs, where the carbon dioxide departs the system. That same
blood, freshly loaded with oxygen, then returns to the left side of the heart through
the pulmonary veins where it enters the second circuit.
2. The systemic circuit uses the oxygen-rich blood to maintain a constant internal environment
around the body’s tissues. From the left side of the heart, the blood moves
through the aorta to a variety of systemic arteries for distribution throughout the body.
After oxygen is exchanged for carbon dioxide, the blood returns to the pulmonary
circuit on the right side of the heart via the superior and inferior venae
cavae (the singular is vena cava).
Although cutely depicted in popular culture as uniformly curvaceous, the heart actually
looks more like a blunt, muscular cone (roughly the size of a fist) resting on the
diaphragm. A fluid-filled, fibrous sac called the pericardium (or heart sac) wraps
loosely around the package; it’s attached to the large blood vessels emerging from the
heart but not to the heart itself. The sternum (breastbone) and third to sixth costal
cartilages of the ribs provide protection in front of (ventrally to) the heart. Behind it lie
the fifth to eighth thoracic vertebrae. Two-thirds of the heart lies to the left of the
body’s center, with its apex (cone) pointed down and to the left. At less than 5 inches
long and a bit more than 3 inches wide, an adult human heart weighs around 10
ounces — a couple ounces shy of a can of soda.
Three layers make up the wall of the heart.
1. On the outside lies the epicardium (or visceral pericardium), which is composed
of fibroelastic connective tissue dappled with adipose tissue (fat) that fills external
grooves called sulci (the singular is sulcus). The larger coronary vessels and
nerves are found in the adipose tissue that fills the sulci.
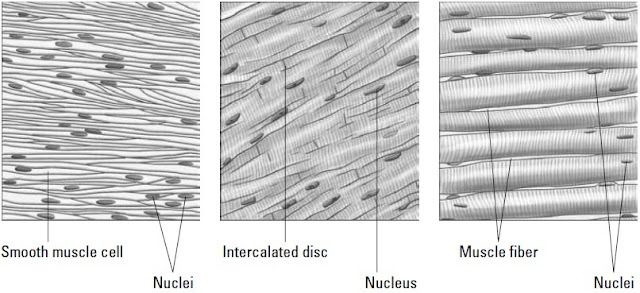
2. Beneath the epicardium lies the myocardium, which is composed of layers and
bundles of cardiac muscle tissue.
3. The endocardium, the heart’s interior lining, is composed of simple squamous
endothelial cells.
Too much to remember? To keep the layers straight, turn to the Greek roots. Epi– is
the Greek term for “upon” or “on” whereas endo– comes from the Greek endon meaning
“within.” The medical definition of myo– is “muscle.” And peri– comes from the
Greek term for “around” or “surround.” Hence the epicardium is on the heart, the
endocardium is inside the heart, the myocardium is the muscle between the two,
and the pericardium surrounds the whole package. By the way, the root cardi– comes
from the Greek word for heart, kardia.
The pericardium is made up of two parts — a tough inelastic sac called the fibrous pericardium
on the outside and a serous (or lubricated) membrane nearer the heart called
the parietal pericardium. Between the serous layers of the epicardium and the parietal
pericardium is the small pericardial space and its tiny amount of lubricating pericardial
fluid. This watery substance prevents irritation during systole (contraction of the
heart) and diastole (relaxation of the heart).
you may also search for:
function of cardiovascular system
cardiovascular system function
human cardiovascular system
cardiovascular system heart
anatomy physiology cardiovascular system heart functions